Idiopathic Pulmonary Fibrosis: A Progressive Lung Disease
 |
| Idiopathic Pulmonary Fibrosis |
Idiopathic pulmonary fibrosis (IPF) is a progressive
lung disease characterized by scarring (fibrosis) of the lungs. The fibrosis
causes the lung tissue to thicken and stiffen over time, making it difficult to
breathe. While the cause of IPF is unknown, it usually affects older adults and
has no cure. In this article, we will discuss what is known about IPF,
including causes, risk factors, diagnosis, treatment options, and research
efforts.
What is IPF?
IPF is a chronic, progressive form of pulmonary fibrosis.
"Idiopathic" means the cause is unknown, and fibrosis refers to the
scarring or damage of lung tissue over time. In IPF, healthy lung tissue is
gradually replaced by scar tissue. The scarring makes the lungs stiff and
thick. As a result, the lungs are unable to circulate enough oxygen into the
bloodstream to meet the body's needs.
While the exact cause of lung scarring is unknown, the damage appears to be due
to an abnormal wound healing process in the lungs after an unknown injury. This
leads to the overgrowth of fibrous connective tissue (scarring) in the lungs.
The end result is stiffness, poor gas exchange, and worsening shortness of
breath over time. IPF usually develops gradually over many years.
Risk Factors and Causes
Some factors may increase a person's risk of developing Idiopathic
Pulmonary Fibrosis, but do not directly cause the disease. These
include:
- Age - IPF typically affects people over 50 and is rare in younger people.
Risk increases with age.
- Gender - IPF affects slightly more men than women.
- Smoking history - Smokers or former smokers have a higher risk of IPF
compared to non-smokers.
- Viral/bacterial infections - Some evidence links certain infections, such as
Epstein-Barr virus and Herpes viruses, to IPF risk.
- Environmental exposures - Occupational exposure to certain metals, wood dust,
silica, welding fumes, and organic dusts are associated with greater IPF risk.
- Genetics - Family history of lung fibrosis may confer increased risk of IPF.
Genetic mutations are linked to a small percentage of cases.
While these factors are associated with IPF, none alone are thought to directly
cause IPF in otherwise healthy individuals. The triggers that induce lung
injury and scarring in susceptible people remain unknown.
Diagnosis and Testing
Since IPF symptoms are similar to other lung conditions, specialized tests are
needed to diagnose IPF. A high-resolution computed tomography (HRCT) scan is
usually the primary test to establish the pattern of lung scarring indicative
of IPF. Pulmonary function tests provide objective measures of lung impairment.
A surgical lung biopsy may be required in some cases to confirm the diagnosis.
The presence of usual interstitial pneumonia (UIP) pattern on HRCT scan or
biopsy is necessary to diagnose IPF with confidence. Presence of other known
causes of pulmonary fibrosis warrants consideration of alternative diagnoses. A
multidisciplinary team discussion, including pulmonologists, radiologists and
pathologists, is recommended to diagnose IPF accurately.
Progression and Symptoms
Once diagnosed, IPF progresses gradually over time. Symptoms worsen as scarring
spreads and more lung tissue is destroyed. Common symptoms include:
- Shortness of breath, especially during activities requiring minor exertion
- Dry cough
- Finger clubbing - enlargement and rounding of the tips of the fingers and
toes
- Fatigue and weakness
As disease progresses, lung function deteriorates and patients experience
increasing breathlessness at rest and reduced exercise capacity. Complications
may include pulmonary hypertension, cor pulmonale, pneumonia, respiratory
failure and death. Median survival is 2-5 years from diagnosis but varies based
on disease severity. Some may live up to 10 years, while others progress
rapidly.
Treatment Options
Currently, there is no cure for IPF. Treatments focus on slowing disease
progression, improving quality of life and reducing symptoms.
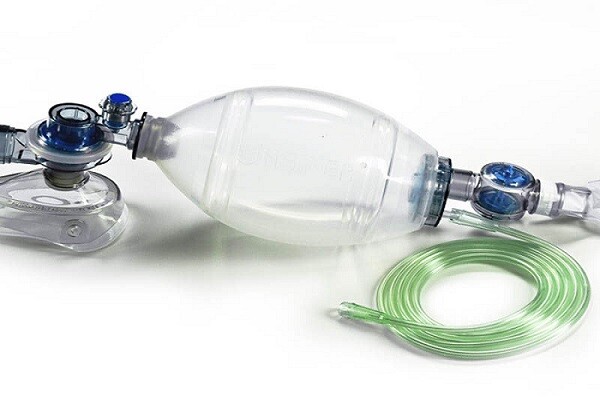
- Oxygen therapy if low oxygen levels are present.
- Pulmonary rehabilitation to improve breathing techniques and exercise
tolerance.
- Lung transplant evaluation for selected patients.
- Medications - Pirfenidone (Esbriet) and nintedanib (Ofev) are the two
anti-fibrotic drugs approved to slow IPF progression based on large clinical
trials.
- Management of complications like pulmonary hypertension if they arise.
- Palliative care to maximize comfort as the disease advances.
- Participation in clinical trials of new investigational therapies whenever
possible.
Research Efforts
Despite current limitations, researchers continue advancing our understanding
of IPF through ongoing basic science and clinical investigations. Areas of
active focus include:
- Identifying environmental and genetic risk factors to allow prevention
strategies.
- Elucidating mechanisms driving aberrant repair responses in the lung to
enable targeted new therapies.
- Developing non-invasive tools like blood tests and breath analysis to better
diagnose and monitor disease.
- Assessing combination therapies and sequential treatment strategies to
maximize benefits.
- Refining assessments of disease prognosis to personalize care.
- Expanding transplant eligibility and post-transplant outcomes through novel
immunosuppressive strategies.
IPF is a chronic, progressive disease affecting the lungs. While its causes
remain unknown, research is advancing our knowledge and management of this
debilitating condition. Earlier diagnosis, combined antifibrotic medication use,
pulmonary rehabilitation, and participation in clinical trials provide the best
approach currently for individuals with IPF. Further discoveries hold promise
to transform IPF care in the future.
Explorer
more information on this topic, Please visit @ https://www.rapidwebwire.com/idiopathic-pulmonary-fibrosis-ipf-growth-demand-and-overview/
Get
more insights on this topic: https://captionssky.com/solar-panel-automatic-cleaning-robot-the-future-of-solar-energy-production/


Comments
Post a Comment